It’s been a minute since I’ve written anything. Been a bit busy. I just looked and I haven’t posted since March 2023! Wow!
Okay, so… We moved to Louisville, Kentucky, in November 2024. Pete actually moved in October 2024, because I stayed behind to deal with the house! I finally just picked up and let our wonderfully amazing realtor, neighbor, and friend take care of things for us. Mindy and Steve are just the most wonderful people. I will for sure miss them the most.
Drove across the country, two dogs and a cat. My sister-in-law, who lives in Wyoming, graciously agreed to keep me company on the trip. We had a pretty good time. Stopped at Devils Tower, Mt. Rushmore, and the Badlands. OH, and Sturgis. It was pretty dead that time of year. But we saw some of the most incredible sights. And we stopped in Indianapolis to see her son, my nephew, for a bit. It was really nice to see him.
We spent 2 months in Airbnb’s with all the animals. That was super fun. I do not recommend. We closed on our house in Montana the same day we closed on the house here. So that was kind of nerve-wracking. We moved in the day before New Year’s Eve. I just wanted to sleep in my own bed! I think we got everything unpacked in less than a week. The house had this bright yellow door. The living room was yellow…I mean YELLOW, the kitchen/dining room was peach. And the bedroom was purple with a silver stripe. It was for sure very colorful. One of the first things we did was have the living room, hall, bedroom, kitchen/dining room, and bathrooms painted. I mean, for the love of all.
Weird being close to family again. Over the holidays, it was very overwhelming. Thanksgiving, my birthday (Pete decided to have a get-together to surprise me), Christmas. I had a family dinner in our house after it was painted and everything. Kind of an open house if you will. But I’m slowly getting used to everything. Weird going from being isolated from town and people all day to living in a neighborhood and having people to do things with.
It was disheartening to leave my DRS in Montana. Very emotional. I have been with them all since the very beginning. Initial diagnosis, the tears, the laughs, the stage IV tragedy. I still miss them like crazy. I have a new team here in Louisville. I have my Oncologist, whom I finally got to smile and laugh a bit. We are still trying to establish a relationship. I have a Cardiologist, because well, the heart thing. I was having heart pains, shortness of breath, and dizziness. Turns out it’s anxiety. I said that, but I guess they need to go through all the things to cover all the bases. I have an Oncology Psychiatrist, primary doctor, a bunch of nurses, and my pharmacy team. I’m going to be getting a Radiology Oncologist here in the next few weeks. But more about that to come.
Trying to learn who does what. Usually, my Medical Oncologist pretty much did it all except a few things. But I think it would have changed a bit had I stayed longer. I was already seeing the nurse most of the time. But the doctor. would always check in on me. It’s for sure a little more corporate here. Everyone has a specific job. Medical Oncologist oversees my cancer and any scans, treatments for cancer. My Onc. Psycharist handles the anxiety meds and keeps me grounded. There is a pain management group I’m in. My cardiologist, of course, is all about my heart and blood pressure, which has been a tad on the high side (shocking). And then my primary doctor, who is an absolute trip. I love him out of all my doctors. He looks at everything and balances everything out. Makes sure overall I’m doing good. He talked to my other doctors to keep everyone in the loop. We just did my cholesterol and well…meh. We also did my A1C. I’ve never had that done before!
Okay, let’s talk about cancer and all the fun. We have reduced my main med (Ibrance) because my white blood cell count has been giving us issues. I’m pretty much going in every other week to get my blood tested to see where we are. I’ve had so many scans: brain, CT, MRI, bone, and heart. I’ve had stress tests, heart monitors for 2 weeks, and I now have a CPAP machine. Evidently, I have sleep apnea, which I don’t snore anymore. So I suppose it’s nice to know I have less chance of dying in my sleep because I stop breathing. We have been playing with anxiety meds and mood stabilizers. I was completely fine with the Lexapro, but they seem to think I have some sort of depression. (News flash! I can’t imagine why.)
My cancer treatment hasn’t changed, just a lower dose of Ibrance; other than that, the same. I’m still doing my Zometa infusions; it seems every 2 months now. But the last time I did my tumor markers, they went up. I was having pain in my hip pretty bad. We did a CT and bone scan. The bone scan was a trip. I’ve never had one like that before. They shoot you up with some radioactive stuff, and you have to wait 3 hours, and then they do the scan. I have learned that during scans, I just zone out and use it to meditate…or sleep if they have my head stabilized. But they are going to zap the lesion on my hip to help with pain and hopefully keep it from growing any more. The reason they didn’t change my meds or are zapping more is because that’s the only one that seems they need to spread the party. Like dude, you have your space, stay in it.
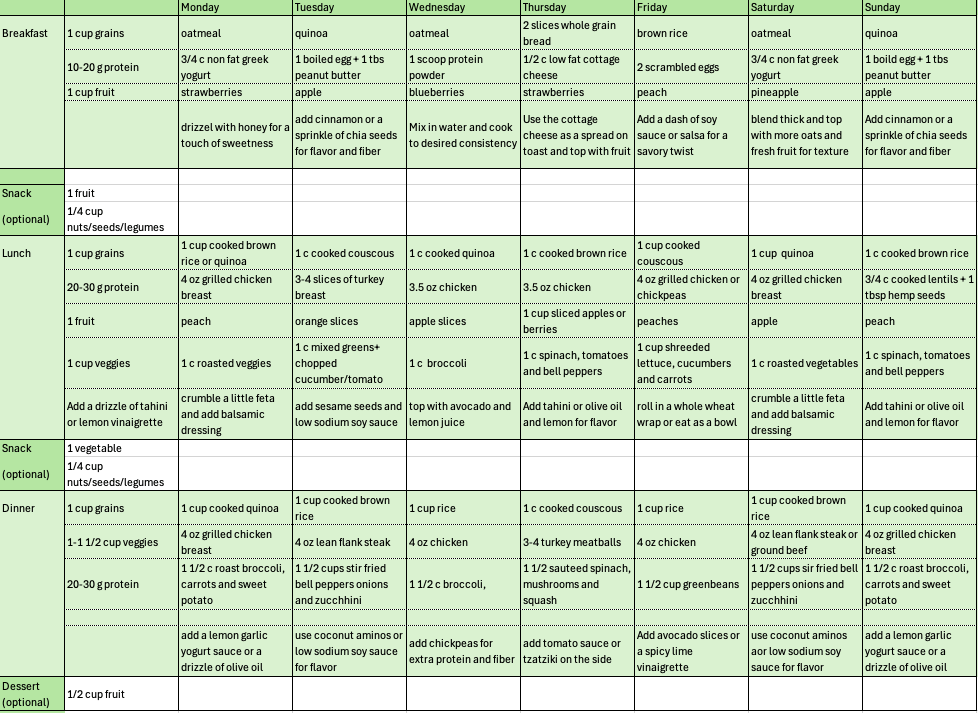
So, yeah. Blood pressure is all over the place. I am on blood pressure meds. Had my cholesterol tested. Total was high. LDL was normal, HDL was high. We will see what they do with that. I’m thinking nothing. And I had my A1C checked. I’ve never had that either. Seems I’m prediabetic. Now, a few weeks ago I met with the oncology dietitian. Oh yeah, I have a dietitian too. She told me how I need to look at eating. Not to worry about calories, but to focus on the food. Basically, every meal should have a protein, a whole grain, and a fruit/vegetable. And of course some healthy fats. She said that this will keep my blood sugar stable, so I don’t go off on some binge. My cardiologist wants me to walk every day. Start low and gradually work up. She said not to worry about distance but time. So start with 10 minutes and every week or so add another 5 minutes. This should all help with my sleep. Did I mention I also have a sleep doctor? I’m going to start making trading cards and collect as many doctors as I can. (ha!)
I have closed my business, shut down all my brilliant ideas (except this one, of course). I’m not doing the magazine anymore. Oh, I was doing the layout for Wedding Planner Magazine for 3 issues, and I just had to stop. That’s a discussion for another time! So my job now is to take care of myself and be happy. I’m getting involved with the cancer community here. And I’m working on a top secret special project that is wonderful because I have no deadlines, and it’s not for anyone but me.
So welcome back to my crazy world!